Women’s Health Interventions
1. Uterine artery (adenomyosis and fibroid) embolization
Uterine fibroids (uterine leiomyomas) are common benign tumors of the uterus that may cause heavy menstrual bleeding, pain, and pressure on the nearby bladder and intestines. Uterine artery embolization (UAE) or uterine fibroid embolization (UFE) is a non-surgical, minimally invasive treatment for fibroids. Fibroid embolization is performed by guiding a small catheter through an artery in the wrist or groin into the arteries supplying the fibroid in the pelvis using real time x-ray imaging (fluoroscopy). Through this catheter, embolization material is injected which blocks off the arteries to the fibroids, causing them to shrink over time. Research has shown that uterine fibroid embolization leads to significant or complete resolution of fibroid-related symptoms in >90% of patients, and surgery (myomectomy, hysterectomy) may be avoided. Prior to undergoing the procedure, it is important to speak with the Interventional Radiologist about any desire for future pregnancy. Typically, patients report mild pelvic pain after the procedure which may be well managed with medications.
Sedation: Local anesthesia (lidocaine) and moderate sedation (fentanyl and midazolam).
Procedure time: 60-120 minutes.
2. Pelvic congestion syndrome treatment
Chronic pelvic pain is common in women and has many different causes, making the diagnosis challenging. Pelvic congestion syndrome (PCS) is one of those causes. PCS results from dysfunctional, dilated ovarian and uterine veins (varicosities) that produce a sensation of heaviness or pain in the pelvis. Varicosities may also be found around the vulva and/or upper thigh. PCS should be considered in women with pelvic pain that worsens with sitting or standing and is relieved by lying down, that worsens during and after sexual intercourse (dyspareunia) or that worsens with urination. Multiple imaging studies may be helpful in diagnosing PCS, including ultrasound (US), computed tomography venography (CTV), magnetic resonance venography (MRV), and pelvic venography. The Interventional Radiologist will also evaluate the risk factors for PCS, imaging results, and symptoms to determine whether pelvic congestion syndrome is a probable cause. The procedure for alleviating pelvic congestion syndrome is non-surgical and minimally invasive. A small catheter is guided through a vein in the leg into the pelvic varicosities using real time x-ray imaging (fluoroscopy). Through the catheter, sclerosants and embolization agents are infused to block the flow of blood into the varicosities. Most patients (>75%) experience relief in symptoms following the procedure.
Sedation: Local anesthesia (lidocaine) and moderate sedation (fentanyl and midazolam).
Procedure time: 60-180 minutes.
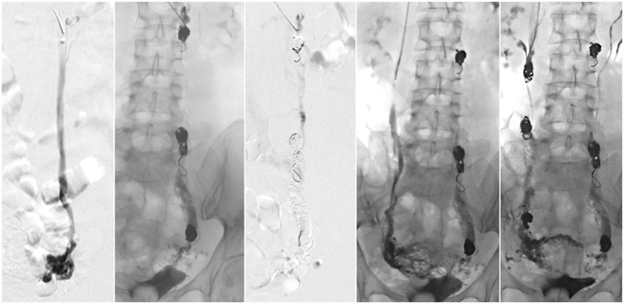
3. Fallopian tube recanalization
Fallopian tube recanalization is a non-surgical procedure for reopening blocked fallopian tubes, a common cause of infertility. The fallopian tubes are part of the female reproductive system and provide a route for the unfertilized egg between the ovary and the uterus. Blocked fallopian tubes are a common cause of female infertility and usually results from a buildup of debris or history of surgery or serious infection. The fallopian tube recanalization procedure is performed by an Interventional Radiologist by inserting a speculum into the vagina and passing a small catheter into the uterus through the cervix guided by real time x-rays (fluoroscopy). Contrast is infused to take a picture of the uterine cavity and the fallopian tubes to identify the location of the blockage. A small wire is threaded into the fallopian tubes to clear away the blockage. In 90% of cases, at least one fallopian tube can be reopened, restoring its function.
Sedation: Local anesthesia (lidocaine) and moderate sedation (fentanyl and midazolam).
Procedure time: 60-120 minutes.