Oncologic Interventions
1. Percutaneous biopsy
A tissue biopsy may be required to diagnose disease. During a biopsy, a needle is inserted through the skin (percutaneous) to collect a sample of tissue using image guidance. The Interventional Radiologist may use ultrasound (US), computed tomography (CT), fluoroscopy (x-ray), or magnetic resonance imaging (MRI) to guide a biopsy device into the target lesion. The tissue sample is then obtained through a special needle and sent to Pathology for testing and evaluation.
Sedation: Local anesthesia (lidocaine) and/or moderate sedation (fentanyl and midazolam).
Procedure time: 30-60 minutes.
2. Tumor ablation
Radiofrequency ablation, microwave ablation or cryoablation are performed by inserting one or multiple small probes through the skin directly into a tumor using image guidance. Tumors in many different organs may be treated with this technique, including the liver, kidney, adrenal glands, breast, bone, lung, pancreas, and thyroid. One or more ablation probes are positioned into the tumor using image guidance. Once the positions of the probes have been confirmed, the tumor is then ablated over a brief period. Radiofrequency or microwave energy is then applied to the probe to heat tissue, destroying the surrounding cancer cells. Tumors may also be destroyed by repeated cycles of rapid freezing and thawing through a procedure called cryoablation. This technique may be preferred over radiofrequency or microwave ablation in select cases. The cryoablation procedure is performed the same way as radiofrequency and microwave ablation. Ablation may be performed as a curative therapy or for symptom relief. Given that this technique is non-surgical and minimally invasive, it is typical that patients return home the day of the procedure, though the care may differ depending on the type and location of the tumor. The Interventional Radiologist will determine which ablation technique is most appropriate for the tumor.
Sedation: Local anesthesia (lidocaine) and moderate sedation (fentanyl and midazolam) or general anesthesia while completely asleep with an endotracheal tube.
Procedure time: 60-120 minutes.
3. Transarterial embolization (TAE)
Tumors grow with the nutrients and oxygen they receive in the arterial blood supply. Embolization therapy for cancer involves the administration of tiny particles (embolization spheres or microspheres) through a catheter directly into a tumor-feeding artery. The goal of bland embolization is to selectively block the tumor blood supply so that the tumor withers and shrinks. Aside from shrinking a tumor, embolization may also be performed prior to the surgical resection of a tumor to limit the amount of bleeding during the operation. Tumors treated with bland embolization are usually located in the liver or the kidney, though tumors in other locations may be eligible for this treatment as well. A small needle will be used to insert a catheter into an artery in the groin or wrist. Using real-time x-ray guidance (fluoroscopy), the catheter will be precisely positioned into one or multiple arteries feeding the tumor. Once positioning of the catheter has been confirmed using x-rays, the embolization particles are injected through the catheter directly into the tumor. Once the embolization has been performed, the catheters are removed, and pressure is held at the needle insertion site in the groin or arm to prevent bleeding after the procedure. Patients may experience self-limiting pain, nausea, and fatigue after the procedure. Most often patients are able to leave the hospital the same day of the procedure or after one night of routine observation.
Sedation: General anesthesia or moderate sedation (fentanyl and midazolam).
Procedure time: 60-120 minutes.
4. Transarterial Chemoembolization (TACE)
Chemoembolization is a minimally invasive cancer therapy proven to be effective in prolonging life in select patients with liver cancer. This procedure may treat tumors that originated in the liver (primary liver cancer) or cancer that has spread to the liver from another organ (liver metastasis). A small catheter is positioned within a tumor-feeding artery, and a mixture of chemotherapy drug and thick oil or tiny particles is administered. A concentrated dose of chemotherapy can be delivered directly into the tumor using this technique. At the same time, the embolization particles block blood flow to the tumor and reduce nutrients and oxygen necessary for its growth. This procedure may be performed multiple times and be integrated into a treatment plan determined by the multidisciplinary cancer treatment team.
Sedation: General anesthesia or moderate sedation (fentanyl and midazolam).
Procedure time: 60-120 minutes.
5. Transarterial Y90 Radioembolization (TARE)
Radioembolization therapy is a palliative or potentially curative treatment for liver cancer. The goal of radioembolization is to infuse tiny particles (microspheres) that contain a radioactive isotope (Yttrium-90 or Y90) directly into the tumor-supplying blood vessel through a small arterial catheter. Because the radiation is locally emitted from within the tumor, radioembolization can safely deliver much higher doses of radiation compared to radiation therapy delivered from outside of the body. TARE requires several separate procedure sessions. First, a mapping angiogram is performed to determine the vascular anatomy and desired radiation dose. Then, the radioembolization procedure takes place 1to 2 weeks afterwards to infuse the radioactive microspheres. Each procedure is performed in an outpatient setting. A small needle is used to insert a catheter into an artery in the groin or wrist after applying local anesthesia (lidocaine). Using real-time x-ray guidance (fluoroscopy), the catheter is precisely positioned into the tumor feeding artery. Once the radioembolization has been performed, the catheters are removed and pressure is held at the needle insertion site in the groin or wrist to prevent bleeding. The procedure is well tolerated with possible self-limited symptoms of fatigue, pain, nausea for several days after. Patients are typically able to leave the hospital the same day of the procedure.
Sedation: General anesthesia or moderate sedation (fentanyl and midazolam).
Procedure time: 60-120 minutes.
6. Transarterial Immunoembolization
Immunoembolization is an emerging treatment for cancer that has metastasized to the liver. The procedure is similar to chemoembolization of liver cancer. A small needle is used to insert a catheter into an artery in the groin or wrist after applying local anesthesia (lidocaine). Using real-time x-ray guidance (fluoroscopy), the catheter is precisely positioned into the tumor feeding artery. Instead of a chemotherapy drug, cytokines are injected directly into the tumor feeding artery to stimulate immune system response against tumor cells. The target vessels are additionally infused with particles to reduce the blood supply to the tumors.
Sedation: General anesthesia or moderate sedation (fentanyl and midazolam).
Procedure time: 60-120 minutes.
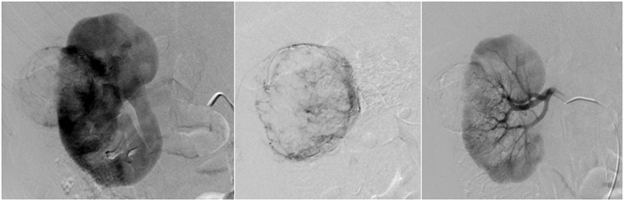
7. Angiomyolipoma embolization
Angiomyolipoma is a kidney tumor composed of blood vessels (“angio”), muscle tissue (“myo”), and fat (“lipoma”). While these tumors are benign, treatment is typically sought because they can spontaneously bleed. They may arise randomly or be associated with an inherited condition called Tuberous Sclerosis. The treatment for angiomyolipomas involves embolization to block tumor blood vessels and prevent rupture and bleeding or to stop bleeding after it has occurred. An Interventional Radiologist performs angiomyolipoma embolization by inserting a catheter into an artery in the groin or wrist after application of a local anesthetic (lidocaine). The catheter is then guided into the renal artery, and contrast is subsequently injected to localize the arteries feeding the tumor. Once identified, the catheter is positioned into the tumor feeding artery before infusing various embolic agents which cut off the tumor blood supply. Once completed, the catheters are removed and pressure is held at the skin insertion site to prevent bleeding after the procedure.
Sedation: General anesthesia or moderate sedation (fentanyl and midazolam).
Procedure time: 30-60 minutes.