Portal Hypertension and Mesenteric Interventions
1. Transjugular Liver biopsy
In patients with diffuse liver disease, a biopsy may be necessary to determine the cause of disease and its severity. Biopsy may be done directly through the skin (percutaneous liver biopsy) or through the jugular vein in the neck (transjugular biopsy). Transjugular liver biopsy is a minimally invasive procedure performed by inserting a catheter into a large neck vein after application of a local anesthetic (lidocaine) and sedation (fentanyl and midazolam). The catheter is then guided into a hepatic vein inside the liver. Then a long, thin needle is advanced into the hepatic vein and surrounding liver tissue using real-time x-rays (fluoroscopy). The biopsy sample is then removed through the catheter in the neck. Pressures in the veins may be measured at the same time if doctors suspected severe liver disease from cirrhosis of the liver or other conditions.
Sedation: Local anesthesia (lidocaine) and/or moderate sedation (fentanyl and midazolam).
Procedure time: 30 minutes.
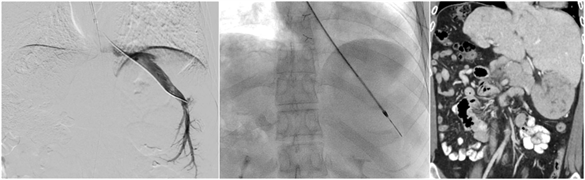
2. Transjugular intrahepatic portosystemic shunt placement (TIPS)
A transjugular intrahepatic portosystemic shunt placement (TIPS) procedure creates an artificial connection between the portal vein and hepatic vein allowing blood flow to bypass the liver. The portal veins carry blood from the intestines and spleen to the liver, and the hepatic veins carry blood from the liver back to the heart. A severely diseased liver (such as in advanced cirrhosis) does not allow blood from the portal veins to flow freely through the liver. This situation increases blood pressure in the portal veins (portal hypertension), which may lead to dilated veins (varices) in the esophagus and stomach that can bleed, abnormal and bothersome accumulation of fluid (abdominal ascites, pleural effusion), or poor kidney function. A TIPS procedure may prevent variceal bleeding or reduce fluid accumulation in the abdomen by bypassing the diseased liver. After a thorough evaluation, the care team will determine if a TIPS is an appropriate treatment option. The procedure is performed by an Interventional Radiologist by inserting a catheter in one of the large veins in the neck after application of a local anesthetic (lidocaine). The catheter is then guided into a hepatic vein in the liver using real-time x-rays (fluoroscopy). Then a specialized needle is passed through the liver and into a portal vein to create a tract that connects the portal vein to the hepatic vein. A covered stent (hollow tube made of wire mesh and covered with fabric) is inserted to keep the connection open. Ultrasound of the liver should be performed routinely to ensure the TIPS stent does not narrow over time.
Sedation: Local anesthesia (lidocaine) and general anesthesia (completely asleep with an endotracheal tube).
Procedure time: 60-120 minutes.
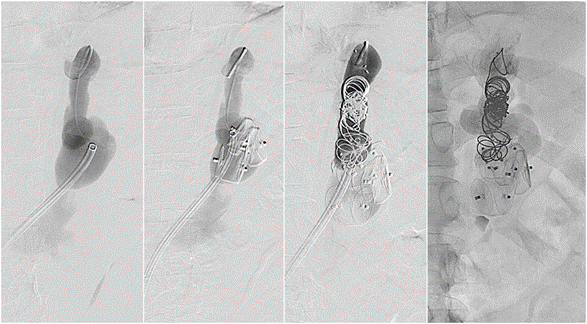
3. Balloon-occluded antegrade (BATO) and retrograde transvenous obliteration (BRTO)
Gastric varices are abnormally dilated veins that may bleed into the stomach. Gastric varices result from portal hypertension, a condition typically associated with cirrhosis of the liver. Balloon-occluded antegrade or retrograde transvenous obliteration (BATO or BRTO) are minimally invasive, non-surgical procedures used to eliminate gastric varices by placing sclerosant and embolic materials directly into the abnormal veins. This procedure may be done separately or in combination with a transjugular intrahepatic portosystemic shunt (TIPS) procedure. The BATO or BRTO procedure is performed by inserting a catheter into a vein in the groin or neck after application of a local anesthetic (lidocaine). The catheter is then guided into the portal vein or renal vein where a small balloon is inflated to isolate the inflow or outflow connections of the gastric varices. With the balloon in place, embolization agents and sclerosing drugs are infused to shut down the gastric varices. Once the procedure is complete, the catheters are removed, and patients often return home 1-2 days after the procedure.
Sedation: Local anesthesia (lidocaine) and general anesthesia (completely asleep with an endotracheal tube).
Procedure time: 60-120 minutes.
4. Splenic reduction embolization
Platelets are blood cells necessary for clotting. Thrombocytopenia is a condition in which the number of platelets in the circulation is very low, increasing the risk for bleeding. In some patients with thrombocytopenia, the spleen traps the platelets from the circulation and becomes enlarged, a condition called splenomegaly. Reducing the spleen size in these patients may return the platelet counts to normal levels. Splenic embolization is a minimally invasive, non-surgical treatment for splenomegaly that can shrink the spleen by cutting off bloody supply to portions of it. The procedure is performed by inserting a catheter into an artery in the groin or wrist after application of a local anesthetic (lidocaine). The catheter is then guided into the splenic artery using real-time x-rays (fluoroscopy). This catheter is then used to administer embolization agents directly into multiple splenic artery branches to reduce functional splenic tissue and thereby increase circulating platelet levels. Once the procedure is complete, the catheter is removed, and patients are monitored in the recovery room. Patients often report some mild abdominal discomfort after the procedure, which can be controlled with medications.
Sedation: Local anesthesia (lidocaine) and moderate sedation (fentanyl and midazolam).
Procedure time: 60 minutes.
5. Portal vein reconstruction
The portal vein carries blood from the intestines and spleen into the liver where it is filtered. In rare cases, the portal vein may become narrowed by an adjacent tumor, due to blood clots, or as a complication from surgery such as liver transplant. In these cases, patients may develop portal hypertension, a condition which may lead to dilated veins (varices) in the esophagus or stomach that can bleed or recurrent abdominal ascites. Portal hypertension may be alleviated by correcting the narrowed portal vein by placing a stent, which is a hollow tube made of wire mesh. Portal vein stent placement is performed by inserting a catheter into the portal vein through the liver or spleen after application of a local anesthetic (lidocaine) and sedation (fentanyl and midazolam). The catheter is then guided into the portal vein and contrast is injected to visualize the narrowing, which is then opened by deploying a stent. Once the procedure is complete, the catheters are removed, and patients may return home after a short stay in recovery.
Sedation: Local anesthesia (lidocaine) and moderate sedation (fentanyl and midazolam) or general anesthesia (completely asleep with an endotracheal tube).
Procedure time: 60 minutes.