Pulmonary Interventions
1. Acute pulmonary embolism thrombectomy and thrombolysis
Acute pulmonary embolism is a potentially life-threatening condition where a blood clot (thrombus) becomes lodged in the arteries of the lung, causing shortness of breath, chest pain, strain on the heart, and low blood oxygen. The primary treatment for a pulmonary embolism is blood thinning medications (anticoagulants). In severe cases of pulmonary embolism, these medications may not be sufficient to rapidly relieve the strain on the heart and lungs. In select cases, an Interventional Radiologist can dissolve or remove the thrombus through a procedure called catheter-directed thrombolysis or thrombectomy. Thrombolysis is a minimally invasive procedure where a catheter is guided into the arteries of the lungs through a pinhole in the neck or groin after application of a local anesthetic (lidocaine). Clot-busting drugs (thrombolytics) are then infused through the catheter positioned directly into the blood clot. Thrombectomy is an alternative or adjunct technique where the thrombus is removed through the catheter, allowing the blood to flow through the lungs again. These procedures are potentially life-saving interventions in patients who are acutely and severely ill from pulmonary embolism.
Sedation: Local anesthesia (lidocaine) and moderate sedation (fentanyl and midazolam).
Procedure time: 60-120 minutes.
2. Chronic thromboembolic pulmonary hypertension (CTEPH) arteriography and angioplasty
When acute pulmonary embolism is incompletely cleared, it may lead to scar tissue formation and obstruction of some of the pulmonary arteries. This is called chronic pulmonary embolism. Chronic pulmonary embolism may cause pulmonary hypertension which leads to shortness of breath, severe fatigue, and heart problems. In patients who are healthy enough for surgery, pulmonary endarterectomy may be performed to remove the chronic clot, which may be curative. However, the operation is high risk, and some patients may not be healthy enough to undergo the procedure. For these patients, there is a non-surgical, minimally invasive option called pulmonary artery angioplasty. This is performed by inserting a catheter into a vein in the neck or groin after application of a local anesthetic. The catheter is then guided into the pulmonary arteries using real time x-ray images (fluoroscopy). A balloon is used to dilate and open the pulmonary arteries affected by the chronic pulmonary embolism.
Sedation: Local anesthesia (lidocaine) and moderate sedation (fentanyl and midazolam).
Procedure time: 60-120 minutes.
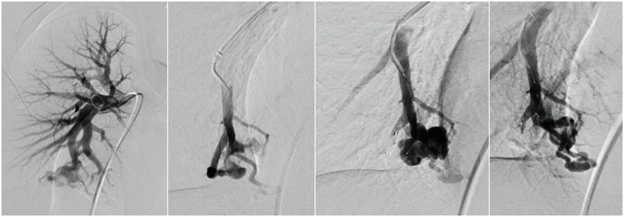
3. Pulmonary arteriovenous malformation embolization
An arteriovenous malformation (AVM) is an abnormal connection between an artery and vein without intervening capillary beds. In the rare situation where one or more AVMs form in the lung, the abnormal communication may allow blood clots to enter arteries feeding the brain, bowel, or kidneys. If left untreated, the most serious risk is the development of a stroke or brain abscess. A minority of patients with pulmonary AVMs have no other underlying medical problems. However, hereditary hemorrhagic telangiectasia (HHT), also known as Osler-Weber-Rendu syndrome, is a genetic condition in which many arteriovenous malformations develop throughout the body, including the lungs. The treatment of pulmonary AVMs by an Interventional Radiologist is minimally invasive and involves guiding a catheter through a vein in the groin or neck into the pulmonary artery using real time x-rays (fluoroscopy). Once the catheter has been positioned into the pulmonary AVM, various embolization agents can be deployed to close off the abnormal blood vessels. Multiple pulmonary AVMs can be treated during one treatment session, and patients typically return home the same day of treatment.
Sedation: Local anesthesia (lidocaine) and moderate sedation (fentanyl and midazolam).
Procedure time: 60-120 minutes.
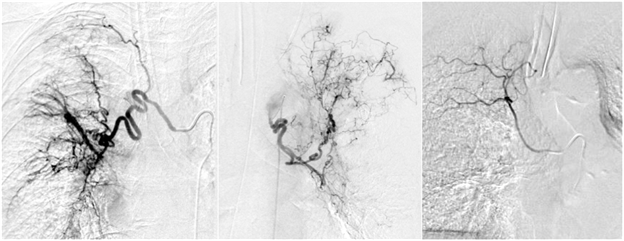
4. Bronchial artery embolization
Conditions including cystic fibrosis, lung cancer and certain infections may lead to bleeding into the airway and lungs (hemoptysis). When severe, hemoptysis may be immediately life threatening or lead to worsening of lung function in the long term. The source of bleeding is usually from bronchial arteries, and these vessels may be blocked (embolization) by an Interventional Radiologist. Embolization of the bleeding artery is performed by inserting a catheter into an artery in the arm or groin after application of a local anesthetic (lidocaine). The internal bleeding is located by computed tomography (CT) and with real-time x-rays (fluoroscopy) with contrast (angiography). A catheter is guided to the bleeding artery using real-time x-rays (fluoroscopy) and embolic agents such as microscopic spheres remain in the hospital for continued close monitoring.
Sedation: Local anesthesia (lidocaine) and moderate sedation (fentanyl and midazolam).
Procedure time: 60-90 minutes.