Venous Interventions
1. Varicose vein endovenous ablation and sclerotherapy
Varicose veins are dilated, tortuous, superficial veins in the arms or legs. Varicose veins arise when veins that are meant to help blood move back to the heart become dysfunctional. When this occurs, blood begins to pool within the veins making them dilated and swollen. Varicose veins may also cause skin irritation, pain, and discoloration. Endovenous ablation is a minimally invasive procedure that heats the vein from the inside out using a small radiofrequency wire under ultrasound guidance using local anesthesia (lidocaine). Radiofrequency ablation is not painful, and the procedure leaves virtually no scars. Once the procedure is complete, the radiofrequency wire is removed, and patients return home the same day. Multiple veins may be treated in a single session. For smaller varicose veins or spider veins, sclerotherapy may be performed. Sclerotherapy is performed by injecting the varicose vein or spider vein with a sclerosing agent which irritates the lining of the veins causing them to collapse and clot. This eventually turns into a scar underneath the skin and the varicose veins fade from view. This procedure also leaves virtually no scar and patients return home the same day.
Sedation: Local anesthesia (lidocaine) and moderate sedation (fentanyl and midazolam).
Procedure time: 30-60 minutes.
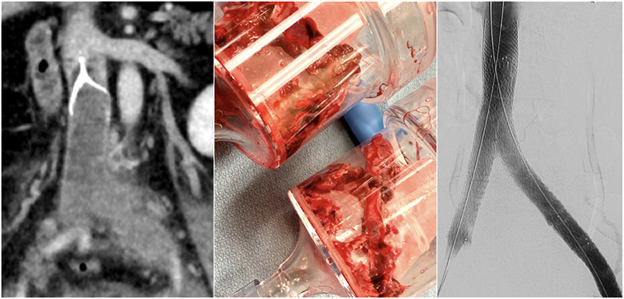
2. Acute deep venous occlusive disease thrombectomy and thrombolysis
Acute deep vein thrombosis (DVT) occurs when a blood clot (thrombus) forms in one or more deep veins of a limb (usually the leg) or the torso and can cause pain and swelling or be completely silent without symptoms. DVT is a serious condition because the clot may break off (embolize) and migrate to the lungs causing a pulmonary embolism, a potentially life-threatening condition. DVT may also damage the involved vein over time, causing it to become narrowed and dysfunctional in a condition called post-thrombotic syndrome. Symptoms of post-thrombotic syndrome include lifelong swelling, heaviness, skin color changes, and ulcer formation which may limit mobility. Blood thinning medications and compression stockings are typically sufficient to treat most acute DVTs. In cases of extensive DVT of the large veins in the thigh and pelvis, blood thinners and compression stockings may not be enough to provide rapid symptomatic relief and prevent post-thrombotic syndrome. In these cases, in addition to blood thinning medications, directly dissolving, or removing the clot may be a better option through a minimally invasive procedure performed by Interventional Radiologists. Catheter-directed thrombolysis is a non-surgical endovascular procedure that infuses a clot-busting drug (thrombolytic) directly into the clot through a catheter that is inserted through the arm, neck, groin, or leg after application of a local anesthetic (lidocaine). Catheter-directed thrombectomy is another non-surgical endovascular procedure that pulls the clot out of the vein through a small catheter that is inserted in the neck, groin, or leg after application of a local anesthetic. Thrombolysis and thrombectomy may be performed in cases of extensive acute DVT to establish faster symptom relief and reduce the risk of developing post-thrombotic syndrome.
Sedation: General anesthesia or moderate sedation (fentanyl and midazolam).
Procedure time: 60-180 minutes.
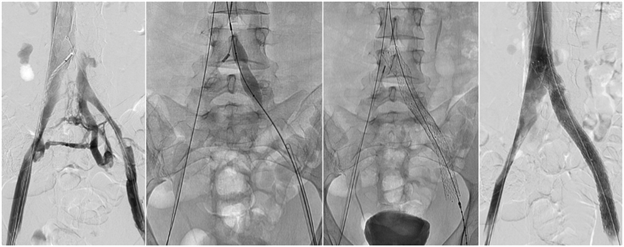
3. May-Thurner Syndrome (Iliac Vein Compression Syndrome) treatment
May-Thurner syndrome, also called iliac vein compression syndrome, occurs when the major artery in the pelvis (right iliac artery) compresses the nearby left iliac vein against the spine. This narrowing of the vein can result in obstruction of the blood flow out of the left leg and may increase the risk of blood clots (acute deep vein thrombosis), tissue swelling, varicose veins, and post-thrombotic syndrome. May-Thurner syndrome is usually diagnosed by the combination of symptoms and findings on imaging studies such as computed tomography (CT) or magnetic resonance imaging (MRI). May-Thurner may be treated by placing a stent (hollow cylinder made of wire mesh) in the compressed area of the left iliac vein to hold it open. This procedure is done by inserting a small catheter into the vein in the groin or neck after application of a local anesthetic (lidocaine). The catheter is then guided to the left iliac vein using real-time x-rays (fluoroscopy) and intravascular ultrasound. Then, a stent is deployed across the left iliac vein compression, allowing blood to flow freely. It is important to continue regular follow-up to ensure the stent remains open.
Sedation: Moderate sedation (fentanyl and midazolam).
Procedure time: 60-120 minutes.
4. Chronic deep venous occlusive disease recanalization and stent reconstruction
Deep vein thrombosis (DVT) occurs when a thrombus (clot) forms in one or more deep veins in the arms, abdomen, or legs. DVT that is present for more than two weeks is considered “chronic.” Chronic DVT forms scar tissues that narrow the inside of the vein and thicken the vein wall. Symptoms of chronic DVT include long-term painful extremity swelling, heaviness, and ulceration of the skin in severe cases. Chronic deep venous occlusive disease may also cause recurrent blood clots in the legs. Compression stockings may provide some relief, but this is not sufficient for some patients. Through a procedure called recanalization and stenting, performed by Interventional Radiologists, the large veins in the arms, chest, abdomen, pelvis, and legs can be reopened, providing significant symptom relief. This is a non-surgical, minimally invasive procedure that involves guiding a small wire through the occluded deep veins and placing stents within the veins to re-establish normal size and course of blood flow. After the procedure, blood thinning medications may help keep the stents from occluding.
Sedation: Local anesthesia (lidocaine) and moderate sedation (fentanyl and midazolam) or general anesthesia while completely asleep with an endotracheal tube.
Procedure time: 60-180 minutes.
5. Extra-anatomic venous bypass creation
The central veins in the chest deliver blood from the head and arms to the heart and lungs. In patients who require multiple catheter insertions in the neck or arms, these central veins in the chest may become damaged and narrowed, leading to swelling and pain in the arm. This may also occur in patients with a fistula in the arm used for dialysis or in patients with a tumor in the chest, breast, or axilla. In rare cases, the damaged veins in the chest cannot be reopened with traditional techniques. In these cases, an extra-anatomic venous bypass may be created through a non-surgical, minimally invasive technique. The goal of the procedure is to create a new route for the blood in the arm to return to the heart, thus relieving pain and swelling. This extra-anatomic venous bypass is created using a wire to create a tract under the skin extending from the veins in the arm to the veins in the neck after application of a local anesthetic (lidocaine) and moderate sedation (fentanyl and midazolam) or general anesthesia. After this tract is created under the skin, multiple stents are deployed to create a new conduit for blood to travel from the arm back to the heart. After the procedure, blood thinning medications may help keep the stents from occluding.
Sedation: Local anesthesia (lidocaine) and moderate sedation (fentanyl and midazolam) or general anesthesia while completely asleep with an endotracheal tube.
Procedure time: 60-180 minutes.