Pain and Palliation Interventions
1. Celiac plexus block and neurolysis
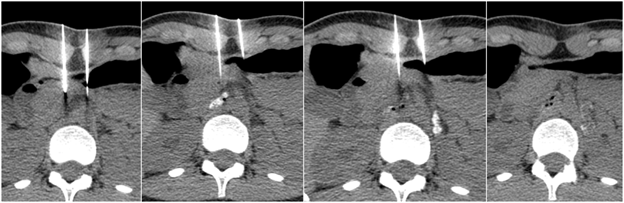
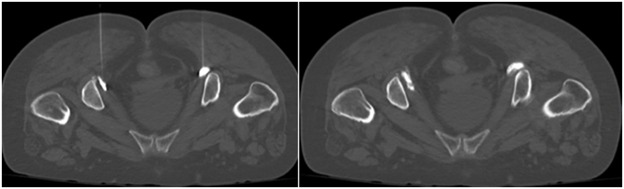
Cancer in the upper abdomen or chronic pancreatitis may cause lifestyle-limiting abdominal pain that may be inadequately managed with pain medications. In these cases, a celiac plexus block or neurolysis may provide symptomatic relief. This procedure may also be completed prior to surgical release for median arcuate ligament syndrome, a condition in which part of the diaphragm impinges on arteries and nerves that supply the stomach and other organs. The celiac plexus is a collection of nerve fibers that are located in the middle of the upper abdomen. These nerve fibers transmit pain signals from the abdomen to the brain. The goal of celiac plexus neurolysis is to disrupt these nerve fibers and prevent the pain signals from being transmitted. The procedure is performed by an Interventional Radiologist inserting a very fine needle through the skin in the abdomen or back into the celiac plexus after application of a local anesthetic (lidocaine). The needle is guided into position with computed tomography (CT) images. Once the needle is in position, a small amount of contrast will be injected to confirm adequate positioning. Then a sclerosing agent will be injected into the celiac plexus, damaging the nerve fibers such that they will not transmit pain signals to the brain. Depending on the results of the first injection, a second needle may be required to ensure the celiac plexus has been well treated. Once the injection is complete, the needle is removed, and CT images are acquired to evaluate the injection site. Most patients experience a reduction in abdominal pain soon after the procedure.
Sedation: Local anesthesia (lidocaine) and/or moderate sedation (fentanyl and midazolam).
Procedure time: 30 minutes.