Fluid Aspiration and Drainage
1. Abscess or fluid collection drainage
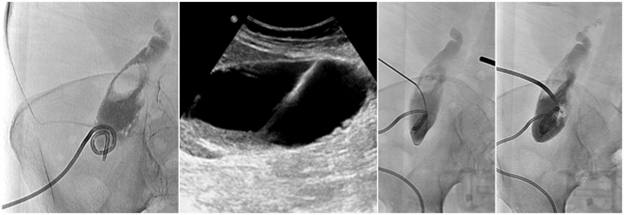
Abnormal collections of fluid can develop in almost any location in the body. Some of the common causes are infection (abscess), bleeding (hematoma) and surgery. Symptoms of abscess include fever, pain, warmth and redness of the overlying skin, night sweats, and elevated heart rate. Antibiotics alone are not sufficient to treat abscesses that are large, due to virulent organisms, or that occur in certain locations. Those collections need to drain through the skin. Fluid collections may be diagnosed by computed tomography (CT), magnetic resonance imaging (MRI), or ultrasound (US). Imaging not only helps to locate the collection but also determine if it can be safely drained by an image-guided procedure. In percutaneous drainage, a needle is inserted through the skin into the fluid using image guidance after the skin has been numbed with local anesthesia (lidocaine). Then, a small drainage catheter is placed into the fluid allowing the contents to drain into a bag outside the body. A sample of the fluid will be sent to a lab for analysis to help tailor the antibiotic therapy. The drainage catheter is then secured to the skin with suture and tape, and the catheter will remain in place until the collection heals. Depending on its size and nature, the catheter may need to remain in place for several days to weeks. Periodically, the drainage catheter must be checked by the Interventional Radiologist using live x-ray imagines (fluoroscopy) to ensure the abscess is healing and the positioning and size of the drainage catheter is optimal. Once it has resolved the drain may be removed by the Interventional Radiologist.
Sedation: Local anesthesia (lidocaine) and/or moderate sedation (fentanyl and midazolam).
Procedure time: 30 minutes.
2. Chest Tube Placement
Abnormal air (pneumothorax) or fluid (pleural effusion) accumulating between the chest wall and the lung surface causes the lung to collapse. This condition may be caused by trauma to the chest, infection, malignancy, heart failure, or for no apparent reason. In most cases, a chest tube (thoracostomy tube) must be inserted through the skin to drain the liquid or air out of the body. The skin is numbed with local anesthesia (lidocaine) prior to the procedure. Chest tube positioning is confirmed using x-ray (fluoroscopy) images. Suction is then applied to the chest tube to evacuate the air or liquid and re-inflate the lung. The chest tube may be removed once the lung heals which typically takes less than a week. Most patients with chest tubes remain in the hospital under close monitoring until the tube may be removed safely.
Sedation: Local anesthesia (lidocaine) and/or moderate sedation (fentanyl and midazolam).
Procedure time: 30 minutes.
3. Chronic Ascites and Pleural Effusion Drainage (Aspira or PleurX)
Ascites or pleural effusion is the buildup of fluid in the abdominal cavity or chest, respectively. There are conditions in which the fluid buildup becomes chronic and recurrent. The result can be shortness of breath or chest pain, or abdominal discomfort and loss of appetite. One option is weekly or monthly drainage through a needle. In selected cases, especially when caused by cancer, an Aspira or PleurX catheter may be placed to allow patients to drain the fluid at home by themselves or with help from a caregiver. The drainage catheter is inserted into the chest or abdomen after application of a local anesthetic using image guidance by an Interventional Radiologist. The outer portion of the catheter is partially tunneled under the skin to protect it against infection. Patients return home the same day after a short stay in recovery and may begin using the catheter immediately. For drainage, the tube is attached to a small reservoir which automatically draws out the fluid. Afterwards, the catheter is disconnected from the reservoir and covered with a dressing.
Sedation: Local anesthesia (lidocaine) and/or moderate sedation (fentanyl and midazolam).
Procedure time: 30 minutes.