Arterial Interventions
1. Acute non-traumatic bleeding interventions and embolization
Acute internal bleeding may result from a variety of diseases. Common sites of internal bleeding include the small or large intestines, retroperitoneum (space surrounding the kidneys), lungs, or the soft tissues of the chest or abdomen. In many cases, bleeding will stop on its own with supportive treatments like blood transfusion and intravenous fluids. In some cases, however, the bleeding is too brisk to be managed conservatively. Embolization is a minimally invasive, non-surgical procedure whereby a small catheter is inserted into an artery in the arm or groin and guided to the site of bleeding using real-time x-rays (fluoroscopy). Once the catheter is in place, contrast may be injected to visualize the bleeding source. Then embolization agents (tiny coils, spheres, glue, plugs, or liquids) are injected through the catheter and plug the bleeding artery. Once the procedure is complete, the catheters are removed, and patients are closely monitored for signs of continued bleeding.
Sedation: Local anesthesia (lidocaine) and/or moderate sedation (fentanyl and midazolam).
Procedure time: 60-120 minutes.
2. Traumatic injury and embolization
Significant traumatic injury may result in internal bleeding in the pelvis, liver, kidney, spleen, or soft tissues. Often, traumatic internal bleeding is sufficiently treated with blood transfusions and intravenous fluids; however, when these conservative measures are not effective, bleeding may be quickly stopped by an Interventional Radiologist with embolization. Embolization of a traumatic bleeding artery is performed by inserting a catheter into an artery in the arm or groin after application of a local anesthetic (lidocaine). The internal bleeding is located by computed tomography (CT) and with real-time x-rays (fluoroscopy) with contrast (angiography). After the bleeding artery is located, a catheter is guided to it using real-time x-rays (fluoroscopy) and embolic agents such as tiny coils or plugs are administered directly into the artery to stop the bleeding. After the procedure, the catheters are removed, and patients remain in the hospital for continued close monitoring.
Sedation: Local anesthesia (lidocaine) and/or moderate sedation (fentanyl and midazolam).
Procedure time: 30-60 minutes.
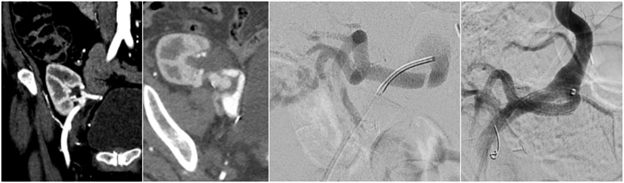
3. Visceral aneurysm repair
An aneurysm is a focal enlargement of an artery that poses the risk of rupture and bleeding. Rarely, an aneurysm may form in the arteries that supply the spleen, liver, kidney, or bowel. These lesions are called visceral aneurysms. Visceral aneurysms most often do not cause symptoms and are incidental findings on computed tomography (CT), magnetic resonance imaging (MRI), or ultrasound (US) imaging. When visceral aneurysms are small, they may be monitored with routine imaging to ensure they do not continue to grow. When visceral aneurysms become too large or grow too quickly, the risk of rupture becomes significant. Certain conditions, such as pregnancy, may cause aneurysms to grow more quickly. Large aneurysms may be embolized (obliterated) or excluded with a covered-stent to prevent aneurysm rupture in the future. Aneurysm embolization or covered stent-exclusion is a non-surgical, minimally invasive procedure that involves inserting a catheter through the arm or groin after application of a local anesthetic (lidocaine). The catheter is then guided into the artery with the aneurysm using real-time x-rays (fluoroscopy). Once the aneurysm is visualized on fluoroscopy with contrast (angiography), a covered-stent is placed across the aneurysm to exclude it from the circulation, and/or tiny coils are deposited into the aneurysm sac to thrombose (clot) the aneurysm and prevent it from expanding. After the procedure is completed, blood is able to flow past the aneurysm and continue on to supply the organ downstream.
Sedation: Local anesthesia (lidocaine) and/or moderate sedation (fentanyl and midazolam).
Procedure time: 60-180 minutes.
4. Acute limb ischemia
Acute limb ischemia is caused by a blood thrombus (clot) that suddenly blocks an artery in the leg causing the leg to become painful, cold, numb, and sometimes difficult to move. In the leg, a clotted artery can prevent blood from delivering oxygen to the lower leg and foot. If left untreated, this condition can lead to permanent nerve damage, amputation, kidney failure, or death. The treatment for acute limb ischemia includes blood thinners, removing the clot blocking the artery, and repairing any defects in the artery that may have caused it. These procedures include catheter-directed thrombolysis and/or mechanical thrombectomy. Catheter-directed thrombolysis is the infusion of a clot dissolving drug (thrombolytic), through a catheter, directly into the artery containing the clot. To perform this procedure, a catheter is inserted into an artery in the arm or groin after application of a local anesthetic (lidocaine). The catheter is then guided using real-time x-rays (fluoroscopy) into the artery in the leg that is blocked by the clot. Clot dissolving drugs are then infused into the artery through the catheter. These clot dissolving drugs may not be enough to re-open the blocked artery in which case a device may be used to pull the clot out through the catheter. After the leg artery is clear of clot, an underlying arterial lesion (such as a plaque) may be identified and repaired by re-opening narrowed areas to allow better blood flow to the legs and feet. Techniques include balloon angioplasty whereby a balloon is inflated within the narrowed area to expand it or stent placement. A stent is a hollow metal tube composed of wire mesh. If a stent is placed, additional medications may be needed to help keep the stent from clotting. Patients usually require a closely monitored hospital stay to ensure the leg heals well and that the arteries remain open.
Sedation: Local anesthesia (lidocaine) or moderate sedation (fentanyl and midazolam).
Procedure time: 60-120 minutes.
5. Chronic peripheral arterial disease treatment (chronic limb-threatening ischemia)
Peripheral arterial disease (PAD) is caused by atherosclerosis of the arteries in the legs. Atherosclerotic plaque builds up in the artery wall and causes narrowing of the vessels which limits the flow of blood and oxygen to the legs. This results in leg pain with walking and in advanced cases may lead to skin ulcers on the legs or feet, leg pain at rest, or the need for amputation. The severity of PAD may be assessed by symptoms and non-invasive imaging or vascular studies. Depending on the extent and location of disease, there are multiple non-invasive procedures that can be performed by an Interventional Radiologist that may improve symptoms when medication and lifestyle modifications are not sufficient. These include angioplasty, stent placement, thrombolysis (clot disrupting drugs). The goal of all these interventions is to re-open arteries that are narrowed or completely blocked to allow better blood flow to the legs and feet, and improve symptoms, mobility, and wound healing. The procedure involves the insertion of a catheter into the arteries of the groin or arm after application of a local anesthetic (lidocaine). The catheter is then guided through the arteries using real-time x-ray images (fluoroscopy) to the site of arterial disease. A small wire is then used to navigate across the area of arterial narrowing. Then a balloon is inflated within the narrowed artery to expand it (angioplasty) which allows blood to flow freely down the leg and foot. Depending on the size and location of the arterial, a stent may need to be placed to keep the artery open. A stent is a hollow metal tube composed of wire mesh. After the procedure, the catheters are removed, and pressure is held at the access site to prevent bleeding. If a stent is placed, additional medications may be needed to help keep the stent from clotting. In cases where PAD is not amenable to a minimally invasive procedure, a vascular surgeon may perform an arterial bypass.
Sedation: Local anesthesia (lidocaine) and/or moderate sedation (fentanyl and midazolam).
Procedure time: 60-180 minutes.
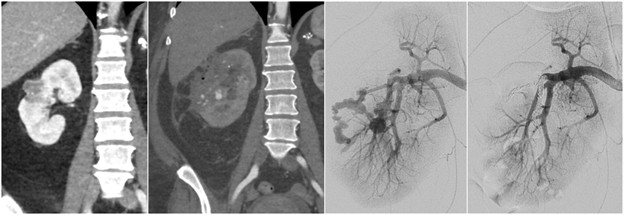
6. Endoleak embolization
An abdominal aortic aneurysm (AAA) is a focal enlargement of the abdominal aorta, the largest artery in the body in the middle of the abdomen. A common, minimally invasive treatment for AAA is endovascular aortic aneurysm repair (EVAR). This procedure involves placing a covered stent inside the aneurysm to exclude the dilated portion of the artery, preventing aneurysm rupture. A covered stent is a hollow metal tube composed of wire mesh covered by fabric. A complication following EVAR is leakage of blood into the aneurysm from around the covered stent or from another vessel in the abdomen (endoleak). Endoleaks may be treated by an Interventional Radiologist using non-surgical, minimally invasive techniques. Once the endoleak has been diagnosed on computed tomography (CT) or ultrasound (US), a catheter may be inserted through the arm or groin after application of a local anesthetic (lidocaine) and sedation (fentanyl and midazolam). This catheter may then be navigated to the source of the endoleak using image guidance (fluoroscopy). Then small coils, glue, or other embolic agents may be delivered through the catheter to seal off the endoleak, preventing the AAA from expanding.
Sedation: Local anesthesia (lidocaine) and/or moderate sedation (fentanyl and midazolam).
Procedure time: 60-120 minutes.
7. Renal artery angioplasty and stent placement
High blood pressure (hypertension) is commonly managed with medications. Patients who are not sufficiently treated with medications may have hypertension caused by a narrowed artery to the kidney, a condition called renovascular hypertension. Renovascular hypertension is the most common cause of secondary hypertension and occurs in 1-5% of patients with high blood pressure. For patients with renovascular hypertension, an Interventional Radiologist may use a balloon to open the blocked artery (angioplasty) or place a stent in the narrowed artery to improve artery blood flow and reduce hypertension. This is a non-surgical, minimally invasive procedure that involves placing a catheter into an artery in the wrist or groin after application of a local anesthetic (lidocaine) and sedation (fentanyl and midazolam). The catheter is then guided into the renal artery using real-time x-rays (fluoroscopy). Contrast is injected through the catheter to identify the site of artery narrowing. A balloon mounted on a catheter is inflated to open the narrowing or a stent is deployed to keep the artery open. After the procedure is complete, the catheters are removed, and pressure is held at the puncture site to prevent bleeding. Patients return home the same day as the procedure after a short stay in the recovery room.
Sedation: Local anesthesia (lidocaine) and/or moderate sedation (fentanyl and midazolam).
Procedure time: 60-120 minutes.
8. Mesenteric ischemia thrombolysis and stent placement
Blood is supplied to the intestines through three arteries: the celiac artery, superior mesenteric artery, and the inferior mesenteric artery. In patients with atherosclerosis, these arteries may become narrowed causing poor blood flow to the intestines. After a meal, the intestines require more blood than the narrowed arteries can supply, causing abdominal pain, nausea or vomiting, and weight loss over time. Chronic mesenteric ischemia may be diagnosed by computed tomography (CT) or ultrasound (US). An Interventional Radiologist may offer a minimally invasive, non-surgical treatment for chronic mesenteric ischemia called celiac artery or superior mesenteric artery stenting. This procedure involves placing a catheter into an artery in the wrist or groin after application of a local anesthetic (lidocaine). The catheter is then guided into the mesenteric artery using real-time x-rays (fluoroscopy). Contrast is injected to confirm the location of arterial narrowing and a stent is deployed to open up the artery. This allows more blood to flow to the intestines and may prevent abdominal pain after meals. After the procedure is complete, the catheters are removed, and pressure is held at the insertion site to prevent bleeding.
Sedation: Local anesthesia (lidocaine) and moderate sedation (fentanyl and midazolam) or general anesthesia (completely asleep with an endotracheal tube).
Procedure time: 60-120 minutes.