Hepatobiliary Interventions
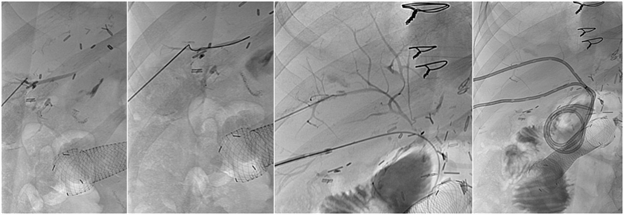
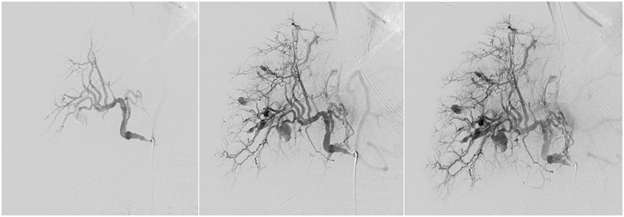
1. Biliary drainage catheters and stent placement
The liver produces fluid called bile which is carried by the bile ducts into the small intestine where it helps digest food and eliminate waste products. Bile ducts may become narrowed due to prior surgery, biliary disease or a nearby tumor. This condition causes bile to back up into the liver resulting in jaundice (yellowing of the skin or eyes) and/or a serious infection (cholangitis). Also, bile ducts may be inadvertently damaged during an operation causing a bile duct leak. In these cases, percutaneous transhepatic biliary drainage (PTBD) may be performed to relieve the obstructed bile duct or prevent further bile leakage from an injured duct. PTBD is performed by inserting a needle through the liver into a bile duct under ultrasound after application of a local anesthetic (lidocaine). A wire is then guided from the bile duct into the small intestine using real-time x-rays (fluoroscopy). Then, a catheter is inserted over the wire, allowing bile to flow freely across obstruction or leakage. This catheter extends from outside the body, across the area of biliary damage or obstruction and into the small intestine, allowing bile to drain into the intestine or outside the body into a bag. In cases where the obstruction or leakage cannot be crossed with a wire, the drainage catheter may be placed to allow drainage of bile outside the body into a bag. Instructions on how to care for the PTBD will be provided, and a follow-up visit should be scheduled.
Sedation: Local anesthesia (lidocaine) and moderate sedation (fentanyl and midazolam) or general anesthesia (completely asleep with an endotracheal tube).
Procedure time: 30-60 minutes.