Soft Tissue Calcifications
<-Periosteal Reaction | Fractures Without Significant Trauma->
Soft tissue calcifications pop up all of the time, and it behooves the radiologist to say something intelligent about them. Fortunately the differential diagnosis for this finding is not too difficult. Soft tissue calcifications are usually caused by one of the following six entities. These are listed below in order of prevalence.
| Differential Diagnosis of Soft Tissue Calcifications |
||
| Cause | Typical Appearance | Prevalence |
| Dystrophic | small to large amorphous Ca++ in the damaged tissue — may progress to ossification (formation of cortex and medullary space are then seen) | 95 – 98 % |
| CPPD | chondrocalcinosis; occasionally associated with calcifications in the soft tissues of the spine | 1 – 2 % |
| Metastatic calcification | finely speckled Ca++ throughout soft tissues | 1 – 2 % |
| Tumoral calcinosis | big globs of Ca++, usually near a joint | << 1 % |
| Metastatic osteosarcoma | amorphous, fluffy, confluent collection of Ca++ | <<< 1 % |
| Primary soft tissue osteosarcoma | amorphous, fluffy, confluent collection of Ca++ | <<<< 1 % |
As you can see, almost every calcification that one sees in the soft tissues in actual radiographic practice is due to dystrophic calcification. What does this mean? Simply this: when tissue is damaged, the body responds to this injury in a nonspecific manner by invoking the generic inflammatory response reaction. This sometimes ends with calcification of the damaged tissue. This calcification is probably usually only microscopic, but is occasionally enough to be seen radiographically.

Patient with dystrophic calcification in the Achilles tendon due to recurrent trauma and tendinitis.
Again, dystrophic calcification means damaged tissue. Any kind of damage will do. Going through the universal differential diagnosis, we come up with the following possible causes:
Mnemonic = VINDICATE
Generic Differential Diagnosis of Dystrophic Soft Tissue Calcifications
- Vascular
- venous insufficiency
- Infection
- Parasitic infestation
- cysticercosis
- dracunculiasis
- armillifer armillatus
- etc.
- Parasitic infestation
- Neoplasm
- primary bone-forming tumor
- osteoma
- osteosarcoma
- tumor necrosis
- primary bone-forming tumor
- Drugs
- Vitamin D
- Autoimmune
- dermatomyositis
- scleroderma
- Trauma
- heterotopic ossification
- injection granulomas
Some foci of dystrophic calcification will go on to actually ossify. The best name for this process (in my humble opinion) is heterotopic ossification (bone formation outside of its usual location). The term myositis ossificans is inaccurate and outdated and should no longer be used. This old term would have one believe that it occurs in muscle (myo-) and is a primary inflammatory process (-itis). In fact, this process occurs not only in muscle, but also in connective tissue. Likewise, any sort of tissue injury can cause heterotopic ossification, not just inflammation.
So, you have just found some white (radiopaque) stuff in a patient’s soft tissue. Now what? Well, before you go too much further, it is nice (in the interests of precision) to decide whether you are dealing with calcification or ossification. If the process of ossification has progressed far enough, this distinction can be made, although this is not always possible. How, then, can one tell them apart? Two key words form the crux of this distinction: order and organization. In bone, calcium is not just randomly deposited all over the place. Instead, it is laid down in a certain orderly pattern. Look for a surrounding shell of dense cortical bone, which surrounds a central medullary space.
Since most calcifications are dystrophic, your biggest job now is to pick the most likely causes of it. The actual morphology of the calcification can help here. For example, consider venous thrombosis. When this occurs around a venous valve, the resulting calcification (or even ossification) is round, dense, and sometimes lamellated, and is called a phlebolith. These are commonly seen in the complex venous plexi in the pelvis. They can also be seen in peripheral veins, especially in the lower extremities. Rarely, one may see them in soft tissue hemangiomas.

Patient with multiple bilateral phleboliths in the pelvic veins.
While parasitic infestations are not exceedingly common, they are around for those who would see them. In our county hospital last year, we saw two patients with cysticercosis just passing across the regular orthopedic trauma board. With parasitic infestations, the morphology of the calcifications can be quite specific. With cysticercosis, the classic findings are multiple elongated foci of calcification just about the shape and size of grains of rice. These “rice grain” calcifications are usually oriented along the direction of the muscle fibers. Dracunculiasis, on the other hand, forms small crescentic calcifications.
Patient with multiple “rice-grain” calcifications in muscles about knees due to cysticercosis.
Following chemotherapy or radiation therapy, a soft tissue tumor may calcify, due to tumor necrosis. In this case, a good history from the clinician will usually provide the answer.
Injection granulomas tend to be focal and densely calcified. They are typically located in common intramuscular injection sites, such as the gluteus maximus.
Autoimmune disorders such as the CREST syndrome or dermatomyositis can also cause soft tissue calcifications. The CREST syndrome consists of calcinosis cutis (usually seen under the skin of the hands or wrists), Raynaud’s phenomenon, esophageal disorders, sclerodactyly, and telangiectasia. In dermatomyositis, the most prominent calcifications are in the muscles of the upper arms and legs.

66 year old male with scleroderma, exhibiting acroosteolysis, skin atrophy over fingertips and calcinosis cutis.


46 year old female with dermatomyositis and extensive soft tissue calcifications about the knee.
Heterotopic ossification can occur almost anywhere in the musculoskeletal system. It is usually seen following focal injury to an area. However, it is also a common complication of closed head injury, paraplegia or quadriplegia. In this patient group, the ossification usually occurs about the shoulders, elbows, or hips.



33 year old female with limited range of motion about shoulder, elbow and knee after closed head injury. Heterotopic ossificiation is noted at all three sites.
Certain patients, such as those with ankylosing spondylitis or DISH (diffuse idiopathic skeletal hyperostosis), have a predilection to form bone around surgical sites. A rare cause of heterotopic ossification is known as myositis ossificans congenita universalis. As the name implies, this entity is congenital and hereditary. It is characterized by profound ossification of the soft tissues throughout the body. This ossification interferes with motion and respiration, and is usually lethal at an early age.
Soooooo….., what about those patients in the other few percent who don’t have dystrophic calcifications. When should you consider these diagnoses? This is not an easy question to answer, but I’ll try.
Metastatic calcifications can result from any process with an elevated calcium-phosphate product. Entities such as renal failure, hyperparathyroidism, sarcoidosis, milk-alkali syndrome, etc. can lead to metastatic calcifications. These are often fine and diffuse throughout the soft tissues.

31 year old female with lupus erythematosus and renal disease, with metastatic calcifications in soft tissues around shoulder and early subchondral collapse of humeral head from early osteonecrosis.
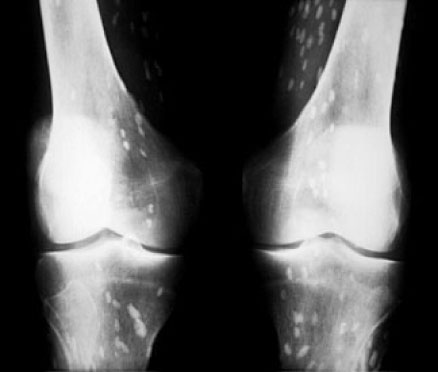
Calcium pyrophosphate dihydrate deposition disease (CPPD) is usually associated with chondrocalcinosis. This typically appears as a fine white line overlying the hyaline articular cartilage. CPPD is also associated with calcifications in the soft tissues of the spine.

Patient with CPPD and chondrocalcinosis of hyaline articular cartilage and meniscal fibrocartilage of knee.
Tumoral calcinosis is a rare, weird entity of unknown etiology. Fifty percent of these patients may have some associated abnormalities in their renal lab work. The calcifications are usually large, globular, and located in the soft tissues over joints. Not much else looks like this.

Elderly female with tumoral calcinosis about hand and wrist.
Calcific tendenitis is commonly seen about the shoulder. The typical appearance is that of small focal globs of amorphous calcification, usually seen around the supraspinatus tendon. These calcifications are in the form of a thick paste of hydroxyapatite crystals.

Patient with a large focus of calcific tendinitis in the supraspinatus tendon.
Osteosarcoma may occasionally metastasize to soft tissue. This is uncommon, and can mimic heterotopic ossification. An even rarer variety of osteosarcoma arises primarily in the soft tissue.

Child with conventional intramedullary osteosarcoma of distal femur with large soft tissue mass exhibiting classic osteoid matrix. However, an osteosarcoma arising from the soft tissues or metastatic to soft tissue would appear much the same as this mass.
References:
- Stewart VL, Herling P, Dalinka MK. Calcification in soft tissues. JAMA 1983;250(1):78-81.
- Resnick D. Diagnosis of bone and joint disorders. 4th ed., Philadelphia, WB Saunders, 2002.