Resident Opportunities
In addition to strong clinical training, our program has numerous educational opportunities including everything from research to global health.
Although not required, many residents choose to take advantage of these opportunities. While many research projects are started organically during clinical work, there is also an Annual Research Showcase to highlight opportunities.
Research
The University of Washington offers abundant research opportunities and our program proudly supports all residents who wish to pursue research.
We offer a research rotation elective – which allows for half days dedicated to research. The other half of the day will be on clinical service, generally in the area of research. To apply for this rotation, residents must submit a brief application regarding their proposed project. Residents are eligible for one research rotation per academic year. Residents who have completed research electives will present at the annual Spring Research Day and many residents also present posters and talks at national conferences, including RSNA, ARRS, and SIR.
Residents Arthie, Jason and Grace at RSNA 2019
In addition to the research rotation elective, we offer a similar educational rotation elective which offers half days of dedicated time to an educational project.
Residents are given 10 professional days each year, which may be used to attend conferences. They do not have to present in order to use this time. First author presenters will be awarded a $3,000 stipend for travel expenses from the Rohrmann Endowment.
There are ongoing Artificial Intelligence projects in conjunction with the deep learning pathway and opportunities for Global Health projects with the global health elective.
In addition, resident quality improvement and quality assurance projects completed during the second or third year of radiology residency may lead to publishable research.
Current and prior residents have won multiple research awards and grants including:
|
|
|
|
Gabriel C. Fine, MD RSNA Research Fellow Grant Research and Education Foundation |
Sana Parsian, MD RSNA Research Fellow Grant Research and Education Foundation |
|
|
 |
|
Ezekiel Maloney, MD NIH T32 |
Marissa Lawson, MD NCI 3DCR T32 training grant |
Deep Learning
The UW Radiology Deep Learning Pathway is an immersive and rigorous experience that trains residents to apply cutting-edge deep learning techniques to medical imaging research. This unique resident training path is the first of its kind to bridge the gap between medical imaging and Artificial Intelligence (AI) education, and was co-founded by former UW resident Mazen Zawaideh, alongside mentors Drs. David Haynor and Nathan Cross.
Deep learning is emerging as a highly promising class of machine learning techniques that allows physicians and engineers to tackle clinical problems that were computationally infeasible just a few years ago. These deep learning methods are setting a new standard in imaging research, and radiologists who are equipped to utilize them will be highly sought after.
In this pathway, residents learn the foundations of deep learning within the domain of medical imaging. The course consists of structured online video lectures, programming assignments, and small-group collaborations. Upon completion, residents will have:
- Understood how to frame clinical problems as machine learning tasks
- Learned to build and train neural networks
- Learned to lead successful machine learning projects as a clinical domain expert
- Applied their knowledge by forming a deep learning team and complete a deep learning project from beginning to end
Upon completion, the resident is awarded a certificate by the UW Department of Radiology to indicate mastery of both deep learning theoretical foundations and practical application in the clinical realm. To learn more, visit www.imagedeep.io
Volunteer Work
Residents are invited to participate in two semi-annual volunteer activities. These are organized by a committee of residents, with prior activities including helping serve at a local soup kitchen, removing invasive plants at local parks, participating in the walk for lupus, and so much more.
In addition to these resident organized events, we also have the unique opportunity to volunteer annually at the Seattle King County Clinic (SKCC). The SKCC is a completely free clinic held in one of Seattle’s largest stadiums! This provides vulnerable patient populations with a wide range of healthcare services, ranging from primary care to mental health and dentistry. This clinic is an amazing way to give back to our community and we are so proud to share that this was created by our very own UW radiologists – Dr. Angelisa Paladin, former Vice Chair of Education and former Residency Program Director and Dr. Norm Beauchamp, Executive Vice President for Health Sciences at Michigan State University and former UW Chair of Radiology.
Global Health
Global health rotations during the PGY-5 year are offered across the world, with flexibility to arrange individualized rotations. These rotations allow residents to learn how radiology is practiced in around the world, while also helping to share our knowledge and improve patient care.
The primary site that residents have gone to in the past is in Naivasha, Kenya. Our program is also very supportive in helping residents to set up global health rotations in their preferred location.
“My Experience as a Radiologist in Naviasha, Kenya” – by Jacob Smith MD, class of 2018
I landed in Nairobi after over 30 hours of travel early on Monday morning with only the name and number of a taxi driver who was supposed to take me from Nairobi to Naivasha, Kenya to where I would be working for the next month. But my cell phone wouldn’t work. I had spoken with AT&T prior to leaving the States and they assured me that my phone would work. But now it wasn’t working. So I sat in the arrivals terminal for about an hour trying to troubleshoot my cell phone situation when a taxi driver with a sign that said “Jack” walked up to me and asked if I needed a ride to Naivasha. “Jack” seemed close enough to “Jake” and he seemed to be aware of the UW and so off we went. That’s how my international rotation in Kenya started this last October. I spent the month working in a county hospital in Naivasha, an agricultural town of about 200,000 people and 100 km from Nairobi. The hospital has 180 beds including both adult and pediatric wards. The care is heavily subsidized by the government and delivered to the poorest citizens of the county. This past year has been especially difficult for the Kenyan government healthcare force. There was a presidential election and in an effort to get better pay and benefits there was a 6-month physician strike followed by a nursing strike leading up to the elections. When I arrived, the nursing strike was still in effect and a skeleton crew was running the hospital. The only internal medicine attending and one of two surgery attendings had left without replacement. Interns, a few mid-level practitioners, and mid-level trainees were essentially running the hospital. As might be expected, limited radiology services are available. Radiology techs are present daily and have a radiography unit and two ultrasound machines. A radiologist from Nairobi comes once a week to review studies, but mainly spends his time reading outpatient radiographs and completes a handful of Doppler ultrasounds. I worked with him each week scanning patients and reviewing cases. I learned a lot about diseases that we don’t see as much of here but are seen on a daily basis in eastern Africa, such as TB, AIDS, and syphilis. The hospital uses a digital radiography unit. However, since they have no hospital network and care is so fragmented, each study is simply burned to a CD. The CDs were then placed into the patient’s chart without an interpretation. Every morning before rounds I would collect the CDs of all inpatient examinations completed the last 24 hours and load them onto a computer. Before rounds I would review the imaging of all their patients with the teams and then round with them. After rounds I would usually take one to two patients to the ultrasound unit to do ultrasounds and help the interns with work on the floor. Thursday and Friday mornings they had formal didactics and they gave me 15 minutes at the beginning of each lecture to teach about radiology. I followed the curriculum of Felson’s Principles of Chest Roentgenology and borrowed heavily from Dr. Rohrmann’s slide sets. These sessions were very well received, as many of the trainees and mid-levels have minimal education and experience with radiology, yet the majority of the studies they order are never read by a radiologist. I also had the opportunity to spend a few days in other settings. I spent a day at an outpatient imaging center in Naivasha where the only CT scanner in town is housed. Additionally, I was able to work at Nairobi’s Kenyatta National Hospital, the country’s largest hospital. It also has the only radiology residency program within the country. I spent time working with their residents scanning ultrasound patients and watching resident read-outs with their attendings. It was a great opportunity to discuss differences in training and learn from them. I am truly grateful to the Rohrmann Endowment and its donors for allowing me to have such an amazing opportunity. It was one of the most impactful experiences of my training. It has given me a different view of medicine and created lasting friendships. I still receive text message photos asking my opinion about studies. I hope that our program is able to continue to support residents in these kinds of projects because these opportunities not only teach us as residents, but also help other clinicians provide better care.
Early Specialization in IR - ESIR
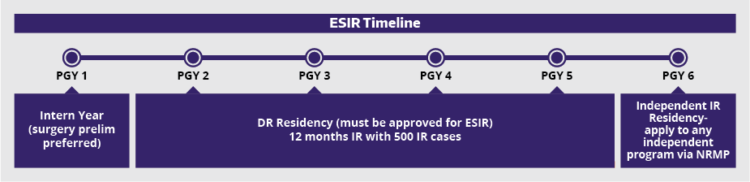
The purpose of the ESIR program is to provide an alternative path for DR residents who identify an early desire to enter into IR. ESIR is a modification of the curriculum of the DR residency and is another option for IR training for some residents.
ESIR training requires a total of 11 interventional radiology or interventional radiology-related rotations (minimum of 44 weeks), and an intensive care unit (ICU) rotation of at least four continuous weeks within the four-year diagnostic radiology residency, with documentation of 500 IR or IR-related procedures. This will allow DR resident to enter the second year of an IR Independent Residency as a PGY-6 and complete the final year of training.
The University of Washington Diagnostic Radiology Residency Program offers Early Specialization in Interventional Radiology (ESIR) in conjunction with the Interventional Radiology Residency Program. Two positions are available for the PGY-4 class each year. The PGY-5 ESIR residents will join the group of seven senior IR residents in their PGY-5 and higher years (Integrated and Independent). The selection committee includes the Diagnostic Radiology Residency and Interventional Radiology Residency Program Directors and Associate Program Directors. Interested residents will submit an updated CV and a letter of interest by December 31 of their PGY-4 year. The committee will make its decision by February 1.
ESIR residents will apply for Independent IR Residency programs through the ERAS/NRMP match, and can apply to their home institution as well as other programs.








