Curriculum
Our curriculum is rigorously reviewed to continue providing current, relevant teaching and experience to our residents while affording them the flexibility they need in their training. Residents will rotate through all subspecialties of radiology and complete their core requirements in the first three years of radiology training.
Clinical Rotations
Residents in the PGY-2 through PGY-4 years have a standardized curriculum with availability for a few electives each year.
Standard rotations at multiple sites include:
- Thoracic radiology including plain film and CT at UWMC and HMC as well as cardiac MR.
- Abdominal radiology including CT/MR rotations at UWMC, HMC, SCCA and the VA.
- Ultrasound rotation includes transplant and, second and third trimester obstetrical ultrasound.
- GI/fluoroscopy rotations at UWMC and HMC including both gastrointestinal and genitourinary studies.
- Body Procedures including ultrasound and CT guided biopsies and drainages
- Emergency radiology at HMC, the only level 1 trauma center in 5 states.
- Breast imaging at SCCA, including tomosynthesis, MRI, and procedures.
- Neuroradiology with CT/MR at UWMC, HMC, and the VA
- Musculoskeletal radiology with plain film, CT, and MRI at HMC and UWMC.
- Pediatric radiology at Seattle Children’s Hospital.
- Interventional radiology at HMC, the VA, and UWMC.
- Nuclear medicine, including cardiac and PET/CT.
In the PGY-5 year, residents have the opportunity to complete 4-6 months of electives, which can be used for in-depth education in more than one field.
Competencies Rotation
With changes in technologies and policies, a radiology program must be able to adapt for the progress of its department and the welfare of its patients. UW Radiology Department is a strong proponent of this ideology and wants to empower the residents to actively engage in this process.
Every resident partakes in a Competencies Rotation based at Harborview Medical Center. This rotation provides residents with two months of dedicated half days to complete a quality improvement project. Each resident is paired with a co-resident in the same class and they will work directly with a mentor within the department to guide them throughout their project development and research.
The residents value this dedicated time as it allows them to delve into meaningful and often surprising issues which, more often than not, result in a progressive change in the residency and department. Several outstanding projects have resulted from this Competencies rotation. Below are some recent examples of our resident projects:
“Contrast Dose Reduction Part II: Lessons Learned from the Shortage and Implications for Future Practice” — Dr. Russel Noh and Dr. Matt Perez
“Screening Mammography at HMC: Stakeholder Perspectives, a Business Case Model, and Suggestions for Improvement” — Dr. Eric Chen and Dr. Nitin Venugopal
“A Review of After-Hours TPS: Lessons Learned and Possible Future Directions” — Dr. Riley Argue and Dr. Andy Guo
“Contrast Dose Reduction: Lessons Learned from the Shortage and Implications for Future Practice” — Dr. Zachary Hill and Dr. Alice Shieh
“Evaluation and Investigation of Interventional Radiology case delays in cases involving Anesthesiology and Interventions for Improvement at a Level I Trauma Center” — Dr. Chase Anderson and Dr. Elizabeth Horneber
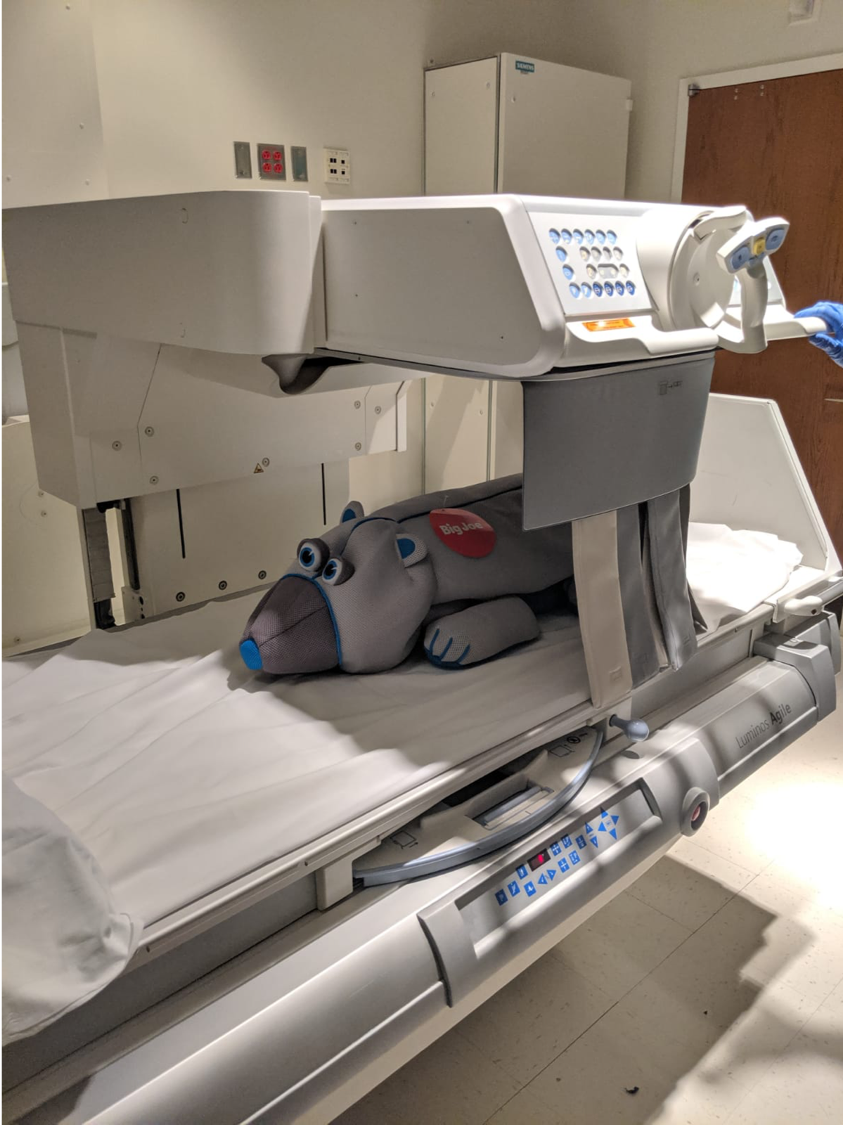
Meet Joe – our very first fluoroscopy patient.
Joe joined the department in 2019 as part of a QI project and helps teach residents about radiation safety.
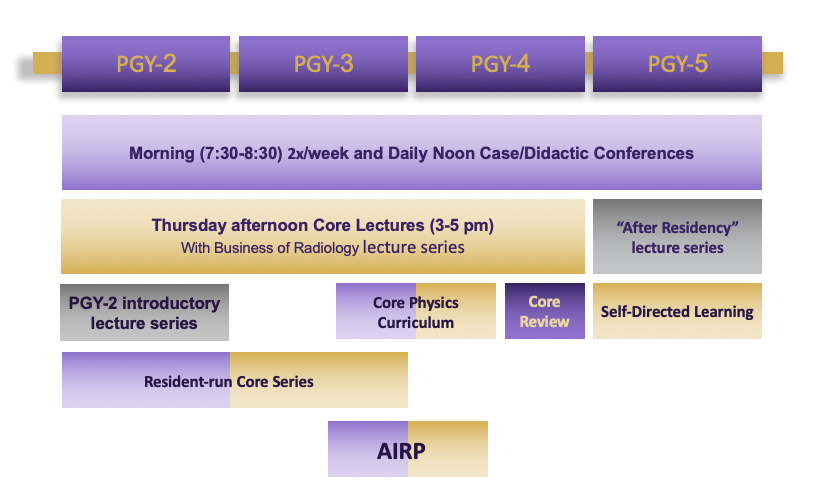
Conferences/Didactics
We have a sound foundation of didactic and case-based teaching conferences. There are daily noon conferences at all sites, with morning lectures at least twice weekly at UWMC.
A series of Core Curriculum lectures are held at UWMC every Thursday from 3-5pm. PGY2-4 residents gather at UWMC-Montlake for in-person interactive teaching sessions for the fourth Thursday of each block. This curriculum covers all subspecialties in radiology.
PGY-2 residents also receive a special introductory course at the beginning of the year, with daily morning lectures. Representative lecture topics include normal anatomy, interpretative approach, dictating an effective radiology report, as well as hands-on sessions at the PACS workstation.
Additionally, our conference curriculum includes a resident-led “Core Series”, which takes place at noon once a week. These lectures are taught by PGY-3 residents and geared towards PGY-2 residents.
Our curriculum also features a comprehensive one-year physics course, taught by the UW Diagnostic Physics faculty. The physics course features topics spanning all of the modalities in radiology as well as radiation safety and biology. The faculty also give a physics board review during the PGY-4 year in preparation for the Core examination.
Our PGY-5 residents participate in the ACR Radiology Leadership Institute Milestone course, which covers education in the Business of Radiology and Healthcare Economics.
Funding (full coverage of course tuition) is provided for all residents to attend the resident four-week ACR Institute for Radiologic Pathology (AIRP).
The PGY-5 class participates in a separate lecture series dedicated to “real world” radiology practice (job applications, contract negotiation, private vs. academic practice, reimbursement models, etc.).
In addition to standardized didactics/conferences, residents also have the opportunity to participate in multi-disciplinary conferences such as tumor boards. Various tumor boards are offered daily at SCCA.
Most conferences have been held virtually via Zoom during the COVID pandemic.
Typical Day
Residents are busy during the workday – interpreting and dictating cases, performing procedures, interacting with patients and referring providers, protocolling upcoming studies, and more. The typical daily schedule varies widely depending on the clinical service, with a sample schedule below:
7:30 – 8:30: Morning conference, didactics and/or case conference
8:30 – 12:00: Assigned clinical service. Alternate between pre-dictating studies and reading out with faculty.
12:00-1:00: Noon conference, didactics and/or case conference
1:00 – 3:00: Assigned clinical service. Alternate between pre-dictating studies and reading out with faculty.
3:00-3:30: Teaching on service with faculty, fellows, and residents sharing interesting cases.
3:30 – 5:00: Wrapping up clinical service. Read out any remaining studies with faculty.
All residents are expected to leave clinical service no later than 6:00pm (usually ~5:00pm on most services) in order to protect resident’s time.