Teaching Files
Archived Case 29
Contributed by: Katherine E. Dee, MD -
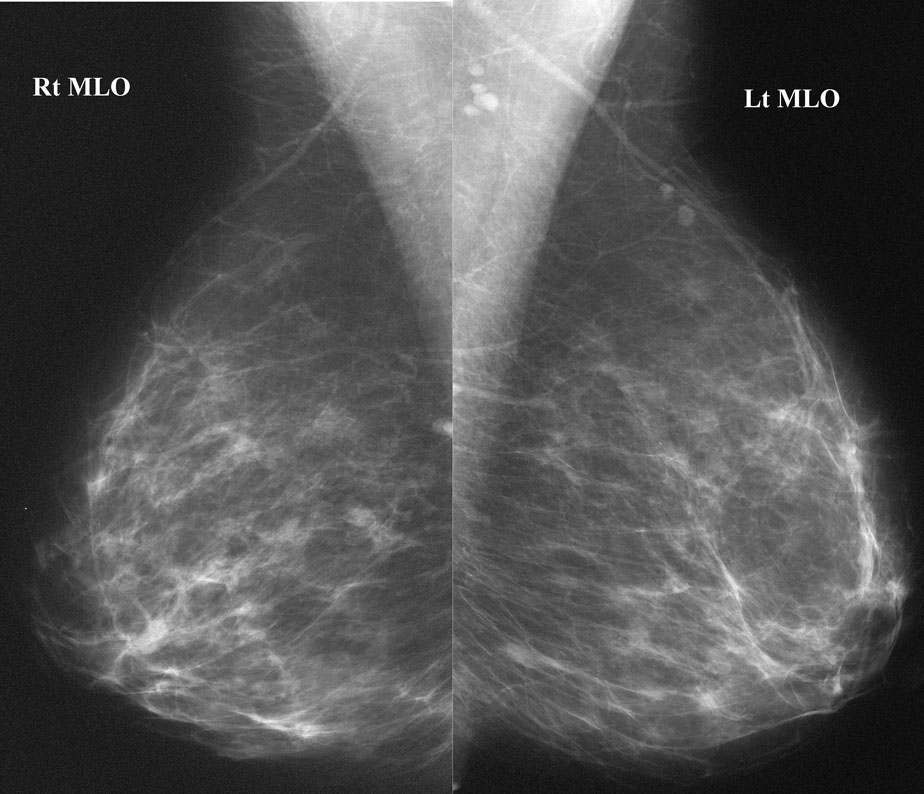
History: Right bloody nipple discharge
What is the next step in the diagnostic work-up?
Spot compression magnification viewsUltrasound
Ductogram
MRI
Central duct excision
OK, that was really the worst trick question in this teaching file so far. You’ll see why
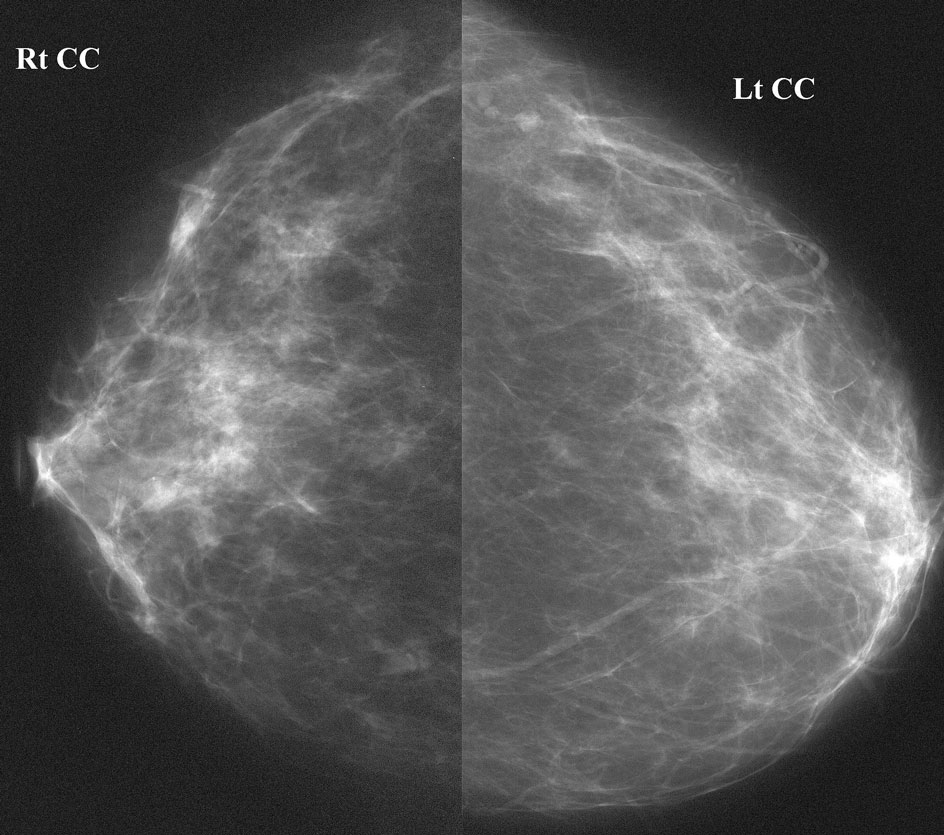
The duct is cut off by a round filling defect. Looking back at the mammogram (click on your browser’s back button), one can see this mass in the retroareolar right breast.
If you had noticed this mass, you would have done spot mags and ultrasound, right? So, if you were so astute, answers a and b are also correct. [BUT, by the way, doing whole breast ultrasound for the work-up of discharge is NOT recommended.]
Some surgeons (especially those who do not have breast radiologists handy) dispense with the ductogram, and recommend central duct excision, since this is the outcome anyway with persistent bloody discharge. (So, if you said answer e, that could also be correct!) However, in most academic centers, ductography is done to localize any lesion prior to surgery, and often surgery is avoided in patients with entirely normal ductograms.
Rarely, one could imagine a case in which persistent bloody nipple discharge might trigger an MRI (answer d) after an entriely negative work-up, but it would not be your next step.
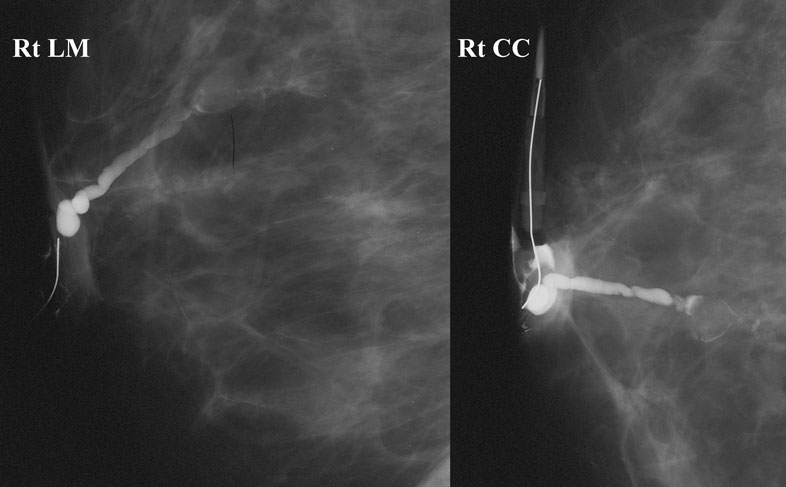
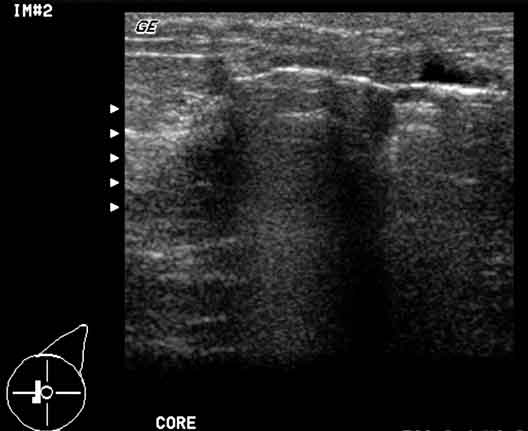
Since we saw this mass on ductogram and mammogram, we thought we’d go ahead and look with ultrasound.
What is your overall assessment?
BI-RADS 2 - Benign - Classic papillomaBI-RADS 3 - Probably Benign - Recommend 6 month follow-up ultrasound
BI-RADS 3 - Probably Benign - Recommend 6 month follow-up mammogram
BI-RADS 3 - Probably Benign - Recommend 6 month follow-up ductogram
BI-RADS 4 - Suspicious - Recommend Biopsy
This most likely represents a papilloma, but any symptomatic solid mass is considered suspicious, and cannot be “probably benign”. Papillary carcinomas and DCIS are occasional causes of bloody discharge.
This patient wanted to avoid surgery at all costs, so we excised the lesion using a Mammotome vacuum-assisted biopsy device. We left a clip at the biopsy site in case any malignant or atypical cells were found.