Imaging Follow Up Safety Net Program enters new phase
By Nathan Cross, MD, MS, CIIP, Vice Chair Informatics, Dept of Radiology
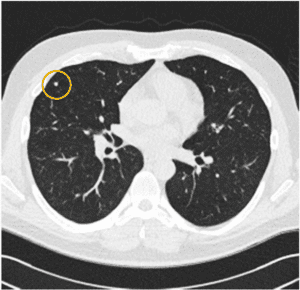
Medical imaging frequently has unexpected findings which can be early indicators of disease. While they may not require urgent workup, ensuring reliable follow up helps us detect diseases early and improve patient outcomes.
Medical imaging frequently has unexpected findings which can be early indicators of disease. While they may not require urgent workup, ensuring reliable follow up helps us detect diseases early and improve patient outcomes.
Every healthcare system has struggled to closely partner with colleagues and our busy patients to ensure appropriate follow up for every follow up imaging recommendation. Given the complexities of modern medicine with patients moving among providers, clinical settings, institutions etc., recommended follow-up can be missed. The Imaging Follow Up Safety Net Program (IFUS) was created to bridge these gaps related to radiology imaging. Begun in 2021 as a pilot program funded through a UW Medicine Patient Safety Innovations Program grant, IFUS staff work with dedicated tools and perform outreach to patients to ensure appropriate follow-up of actionable radiology findings.
Several patients who were at risk of delays in diagnosis and subsequent treatment are receiving care today due to IFUS intervention. One example is a patient who had an outpatient MRI due to unrelenting back pain; this demonstrated incidental lymphadenopathy, for which a follow-up CT was recommended. The patient’s primary care provider noted this recommendation but, due to challenges with care coordination, the CT was not scheduled until the IFUS team contacted the care team. This resulted in completion of the recommended CT, a subsequent biopsy, and a diagnosis of chronic lymphocytic leukemia (CLL). Were it not for IFUS, this patient would otherwise have likely missed follow up until the CLL was symptomatic.
Despite the substantial impact, the IFUS process is simple. When radiologists discover imaging that requires follow-up, they add it to the IFUS queue for monitoring. This allows nurse navigators to review the case and ensure that the recommended follow up occurs in the specified time frame. Navigators do not remove the case from the queue until the recommended follow up is complete. If the follow up imaging does not occur, the navigator contacts the provider, patient, family, or outside provider, depending on the situation.
An IFUS pilot on a small sample of recommendations proved to be successful, increasing follow-up rates from 55% to 77.4%. Due to the success of the program and the support of UW Medicine, Harborview Medical Center, UW Medical Center, and Fred Hutch Cancer Center (FHCC) leadership, the first full time nurse navigator was hired in 2023, and the program scope expanded to include FHCC patients. The program continues to grow, supporting more patients and providers. In 2024, an additional nurse navigator was hired, and new automated software will be implemented that will allow the program to capture significantly more recommendations and, with the help of additional team members, all recommendations will be monitored to prevent delays in care to our patients, friends, and colleagues.
Project contributors include:
Erin Aas, MSN, ARNP, CPHQ, Project Co-Leader, Director of Quality Improvement, Assistant Administrator HMC
Nathan M Cross, MD, MS, CIIP, Project Co-Leader, Vice Chair Informatics, Dept of Radiology
Ali Gould, RN, MHA, Health Program Ops Specialist, Project Nurse Navigator
Scott Andrews, RN, Project Nurse Navigator
Manjiri Dighe, MD, FSAR, FSRU, Vice Chair of Quality and Safety, Department of Radiology
Rekha Matken, Assistant Administrator, Interventional Radiology
Karen Ordovas, MD, MAS, Chief, Cardiothoracic Imaging Section
Dawn Vincic, Associate Administrator Essential Services, Radiology & Radiation Oncology
Dushyant Sahani MD, Chair, Department of Radiology
Martin Gunn, MBChB, FRANZCR, FASER, Sponsor
Kris Bakke, Radiant Lead Application Analyst
Katie Kowalski, MN, ARNP-C, Department of Radiology
Tom Gallagher, MD, MACP, Professor and Associate Chair, Department of Medicine
Timothy H. Dellit, MD, CEO, UW Medicine, Executive Sponsor