Radiology Doctors Volunteer for Global Health Experience in Tanzania
Earlier this year, Blaine Menon, MD, and Kara Fitzgerald, MD, Interventional Radiology (IR) Integrated Residents, had the unique opportunity to travel to Tanzania with Road2IR. Blaine participated in the department’s Global Health elective, and Kara joined him for a week as a volunteer. UW Radiology IR attending doctors Jeff Chick and Matthew Abad-Santos also volunteered with them.
THEIR STORY
“Located in sub Saharan east Africa, with a population of 455 million, Tanzania has a population of about 60 million people within about 130 different tribes. We went to Dar es Salaam, the largest city in Tanzania. It is the finance capital with about five million people.

This is the most densely populated area along the Indian Ocean; almost 50% of their population is 18 and under. Physician density and hospital bed density is far lower than in the US. HIV prevalence is 4.5%. While there has been a lot of progress with improvement in quality of life and access, about one-quarter of the population live on less than the equivalent of 21 US dollars per month. They do not have good access to electricity, water, or sanitation.

We traveled to the hospital network and university area called Muhimbili University of Health and Allied Services (MUHAS), Tanzania’s main medical academic teaching center. The campus is comprised of four institutions. The hospital is a 10-minute walk, where we had to go to the angio suite. Most of the area was open to the outdoors – an open air campus including the waiting area for the radiology area.
 Road2IR is a nonprofit with the goal to build self-sustaining IR training programs in East Africa. When it was first started, a needs assessment in 2017 revealed only one IR physician in Tanzania for 60 million people, no regional training program and a few training programs in Africa but nothing close to what was needed. In 2018, they wrote an Radiological Society of North America grant and were awarded $70,000 to start the program and worked to create a Masters in Science program, equivalent to a fellowship, which was started in 2019. Currently they are starting up programs in Rwanda and Uganda.
Road2IR is a nonprofit with the goal to build self-sustaining IR training programs in East Africa. When it was first started, a needs assessment in 2017 revealed only one IR physician in Tanzania for 60 million people, no regional training program and a few training programs in Africa but nothing close to what was needed. In 2018, they wrote an Radiological Society of North America grant and were awarded $70,000 to start the program and worked to create a Masters in Science program, equivalent to a fellowship, which was started in 2019. Currently they are starting up programs in Rwanda and Uganda.
 Radiology at MUHAS is ultrasound heavy; however, they have received a lot of donated equipment and they have an MRI and CT and a robust residency with 25 residents. Neuroradiology curriculum is taught by US faculty who broadcast lectures and come over, and residents do abroad rotations in the US.
Radiology at MUHAS is ultrasound heavy; however, they have received a lot of donated equipment and they have an MRI and CT and a robust residency with 25 residents. Neuroradiology curriculum is taught by US faculty who broadcast lectures and come over, and residents do abroad rotations in the US.

The IR department is new. They were able to acquire a room and refit it for their needs. It has a small desk and projector, and patients sit in the room for consultation; it also functions as a place for morning conferences for doctors.

About the IR layout at MUHAS: they have a CT procedure suite. On the right is the angio suite at the hospital we had to walk 10 minutes to. The C-arm and ultrasound suite with beautiful designs make you feel like you are outside.
One of the most exciting things that happened while we were there was that the prior week they were able to build a new angio suite in their hospital. This was much more than giving access to a room. As a department they had to pay to use the other angio suite. With the support of the hospital they were able to open their own angio suite.
 IR supplies are difficult to obtain. The supply chain is difficult to navigate. Everything is donated! They have very few workhorse-type items. They use things we would never think about using here, but they are wonderful at working with what they have. For one case, all the transhepatic biopsy devices were failing and they had to try many different ones. To get the devices for your case, everything is donated so there is a huge room where things are hung up on the wall and you don’t know how much of what you have. The fellows collect all the supplies they need the night before, load them up on a box on a wheelchair and push them over to the angio suite.
IR supplies are difficult to obtain. The supply chain is difficult to navigate. Everything is donated! They have very few workhorse-type items. They use things we would never think about using here, but they are wonderful at working with what they have. For one case, all the transhepatic biopsy devices were failing and they had to try many different ones. To get the devices for your case, everything is donated so there is a huge room where things are hung up on the wall and you don’t know how much of what you have. The fellows collect all the supplies they need the night before, load them up on a box on a wheelchair and push them over to the angio suite.
The IR trainees – two graduating classes, three fellows in each graduating class – get paired with a junior and a senior. The Masters of Science in IR is not a job like here, it is more like a masters program that you pay for to get the training. It is quite a sacrifice to get their career started.
Thanks to a recent donation they received a research stipend to help offset the costs. The curriculum is didactic and case-based and covers the full gambit of IR over two years. They do a lot fewer procedures than we do here, about 200-300 before graduating, but more than enough non-vascular procedures. They are rapidly growing their vascular service line and are seeing an increase in angioplasties and embolizations.
 We worked with an amazing group of attendees who graduated from the program, from the first graduating class. The program is also supported by faculty from around the world. Attendings from Germany arrived a couple of weeks before us and we coordinated our trips. Our faculty members, doctors Chick and Abad-Santos represented the UW, with both of them volunteering for their first time with Road2IR. IR attendings are the backbone of the entire program. There are also residents in training and other medical students and pre-med students.
We worked with an amazing group of attendees who graduated from the program, from the first graduating class. The program is also supported by faculty from around the world. Attendings from Germany arrived a couple of weeks before us and we coordinated our trips. Our faculty members, doctors Chick and Abad-Santos represented the UW, with both of them volunteering for their first time with Road2IR. IR attendings are the backbone of the entire program. There are also residents in training and other medical students and pre-med students.
 There are a lot of educational activities and a very robust research program. Here is an example of IR ingenuity at MUHAS. A lot of problems come up when you try to do IR in this setting – how do you deal with a sterile field when you don’t have all the disposable supplies you need? There are no sterile ultrasound covers. So, they made a custom reusable sterile cloth and gloves that are not often used (such as those too large or small) to cover the end of the probe and they use betadine instead of sterile ultrasound gel. They are able to get amazing images due to their ingenuity!
There are a lot of educational activities and a very robust research program. Here is an example of IR ingenuity at MUHAS. A lot of problems come up when you try to do IR in this setting – how do you deal with a sterile field when you don’t have all the disposable supplies you need? There are no sterile ultrasound covers. So, they made a custom reusable sterile cloth and gloves that are not often used (such as those too large or small) to cover the end of the probe and they use betadine instead of sterile ultrasound gel. They are able to get amazing images due to their ingenuity!
We met each morning. The fellows go over cases for the day, and in between cases, clinic happens. Sometimes patients and their families walk through the door with a CD containing images. They project them on the wall and talk to the patients in real time and come up with a plan, one consult at a time.

The rest of the day was spent in cases. The IR group has done an amazing collaboration with the hepatobiliary surgeons, providing biopsies and diagnosing cases, including therapeutic options.
One case we worked on while there (and this is common): a dialysis patient comes in. A lot of patients do not have access to care and end up with arteriovenous fistulas. They have central lines in for a long time and this ends up scarring their veins. A lot of the work is trying to open up veins.
Another type of patient is young women who have locally invasive cervical cancer. Before IR came about, they would come to the hospital, but would be sent home to pass with their families. They were coming in with renal failure and they were not able to do anything for them. A simple nephrostomy tube helped their renal function improve. Now, the oncology service is able to offer them things they were not able to offer before, such as chemotherapies.
 Kara and I also got involved with peer-to-peer teaching, which was an amazing experience. There was so much to learn from them and so much to teach. We had more formal teaching sessions with in-service on devices, and hands-on demonstrations. The group was excited to get to know how to use the devices. Also, important thing to note – they were amazing hosts and helped us to choose the right foods and snacks!
Kara and I also got involved with peer-to-peer teaching, which was an amazing experience. There was so much to learn from them and so much to teach. We had more formal teaching sessions with in-service on devices, and hands-on demonstrations. The group was excited to get to know how to use the devices. Also, important thing to note – they were amazing hosts and helped us to choose the right foods and snacks!
Another main thing we spent our time on outside of patient cases was helping them build a simulation lab. They don’t see the same number of cases we see here and they experience gaps when attendings cannot come and they still want to teach their fellows. In collaboration with faculty at Yale we helped them apply for an RSNA International Education Scholar Grant.
We reached out to Simbionix and asked if they would partner with us. They agreed to donate an AngioFlex simulator device to Road2IR. They are building a curriculum for that. We also got involved in low fidelity simulation, using vascular access phantoms. The junior fellows enjoyed working with us. They do not get a lot of exposure to vascular access early on.
Another project was the Oculus 3D Video library from Yale, a video library of procedure trainings. Fellows can watch these videos using the device, and it feels like you are in the procedure room. It is a great way to prep for the procedure.
Dr. Wayne Monsky helped Blaine with this project – he connected us with Dopl Technologies. We met in a virtual environment and had on the Oculus devices. They handed Blaine the controls to a robot-guided catheter in Seattle and he was able to move it in its virtual environment and it was in real time. Using this as a proof of concept, this simulation can be used over a distance.
We are so excited that folks are interested in continuing some of this work. All three PGY-3 IR residents are interested in going to Tanzania or Rwanda and working on more low fidelity simulation work. As for future projects, we are hoping to be able to get some endovascular models and the fellows will be able to use those for training. We are also hoping to get a handheld ultrasound device for phantoms.

IR GLOBAL HEALTH – WHY WE WENT THERE
Blaine: Today millions lack access to essential and life-saving procedures. There is no doubt the work that was done was essential for those patients. We have the opportunity to create an impact that is much larger than we can see, as the fellows continue to train others. There were many opportunities for personal and professional growth, because of the connections I made with the people I met.
Kara: We got to be there where it was fully immersive, growing ourselves, growing with the residents. It was great to see how many women are having wonderful opportunities as trainees and becoming IR attendings, or as nurses or techs helping. The economic advancement is huge, with more opportunities for folks, and women specifically. More residents will be traveling, and we always need more support for future trips. Also, volunteering to do lectures can be beneficial to IR residents.
You can learn more about Road2IR by following them on Instagram or X (formerly Twitter) or by listening to their stories.
Thank you all for your support. We are grateful and excited for the residents who will continue the work.”
– Blaine Menon, MD and Kara Fitzgerald, MD
Doctors Menon and Fitzgerald shared their experiences at the Sixth Annual Radiology Lunch and Learn Event. You can view their presentation on YouTube [starts at minute 26:27].
Additional thanks to the Rohrmann Endowment, which provided support for this educational opportunity.
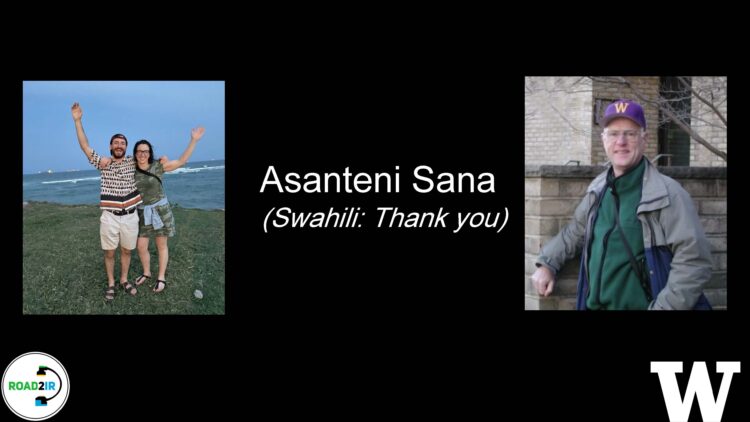
Doctors Blaine Menon and Kara Fitzgerald are pictured together left, and Charles A. Rohrmann, Jr. M.D. is on the right.